Symptoms that develop post-infection are not always due solely to the infection itself. Hospitalization for any reasonincreases a person’s risk for a wide range of medical problems after discharge. Such problems may have little to do with the initial diagnosis and instead stem from the stress of a hospital stay: The disrupted sleep, poor nutrition, and lack of exercise can all contribute to the onset of new health problems. Additionally, people who are very sick do not always fully recover, and their lingering symptoms are often not specific to the initial illness.
“We have names for those syndromes already,” including post-intensive care syndrome and post-hospitalization syndrome, said Anil Makam, a hospital medicine physician at the University of California, San Francisco, who studies patients in long-term acute care hospitals, where many patients go after an ICU stay. Makam recently published a studythat used validated surveys as well as interviews to understand the long-term outcomes of patients who were hospitalized with the most severe cases of Covid-19. His study didn’t have a control group, he said, but the results echo what was known before the pandemic: The sicker the patient, the more likely they are to have persistent multisystem disabilities.
It doesn’t make sense to conflate these conditions with long Covid, he said. Lumping everything together leads to a distorted view of long Covid, and it could complicate efforts to understand the underlying mechanisms and identify possible interventions. “You’re just going to be on a wild goose chase to find treatments,” he said.
Some experts said a broad definition could be useful in the context of public health and epidemiology. Sharon Saydah, an epidemiologist at the Centers for Disease Control and Prevention, said that when CDC scientists crafted the agency’s long Covid definition, they wanted “to make sure we’re not missing anything, that we’re including everyone who might be experiencing ongoing symptoms or new conditions” related to a Covid-19 infection. In a 2021 opinion piece for The Guardian, Al-Aly criticized the WHO’s definition for excluding new onset diseases, such as diabetes and heart disease, which his own studies have detected. These new conditions should count as long Covid, he wrote; otherwise, governments may fail to prepare for “the tide of patients with these chronic conditions.”
(In an email to Undark, a WHO spokesperson, Tarik Jasarevic, wrote that its definition may include new onset disease: The definition “focuses on symptoms but doesn’t specifically exclude new onset disease. New onset conditions like diabetes, lupus, stroke, etc. may be considered” long Covid, Jasarevic wrote.)
At stake, Al-Aly suggested, is a broader struggle: That of long Covid patients who seek to have their symptoms taken seriously, but may encounter skepticism from peers, employers, and caretakers. “I worry that this myopic definition of long Covid may be used by governments and health insurers to debase the disease and deny insurance coverage,” he wrote. “It may add fuel to the gaslighters’ fire, providing them with a moral license to sow more skepticism around the existence of this disease.”
In an interview with Undark, he said that for too long post-infectious illnesses were marginalized. Then, when pandemic hit, the health care system was caught flatfooted. There is no national medical society to champion patients’ cause, and individual physicians are unsure about how to help, he said. Congress allocated more than $1 billion in 2021 to fund long Covid research (and the government kicked in an additional $515 million this year). That’s a start, said Al-Aly. But it’s nowhere near enough.
In the spring of 2021, after Nature published Al-Aly’s first long Covid paper, Anders Hviid’s first reaction was surprise. Nature is a top journal, but it was unusual for the publication to feature epidemiology, said Hviid. Even more unusual were the study’s findings. “It’s just difficult to imagine that a simple respiratory virus could be so detrimental to all organ systems at a population-level scale,” said Hviid. One’s intuition can always be wrong, he added, but given that other respiratory infections, including influenza, do not exact such a massive toll, skepticism seemed like the right starting point: “You should question, ‘Can that be right?’”
For more than two decades, Hviid has conducted research using Denmark’s centralized medical records. During the pandemic, he and his colleagues used electronic health record data to conduct vaccine safety and effectiveness studies. And by late 2020, he had also turned his attention to long Covid, securing funding for a study that would survey the Danish population about their post-Covid symptoms. Such questionnaires offer fine-grained data that can be difficult, if not impossible, to obtain through electronic health records, said Hviid. Nevertheless, Al-Aly’s study had piqued his curiosity. He decided to conduct EHR-based studies as well.
This February, he and four colleagues published a study using medical records of the entire Danish population aged 12 and over. In contrast to Al-Aly’s work, that study found no evidence of substantial neurological or psychiatric symptoms in non-hospitalized individuals one year after a Covid-19 infection.
A defining feature of the study, said Hviid, is its high number of mild or asymptomatic infections. These were documented thanks to the country’s widespread surveillance testing. People getting tested in Denmark were often young and healthy. They got tested because it was a requirement for socializing.
Hviid’s team did see a meaningful increased risk of persistent symptoms among those who had been hospitalized. “That’s not particularly surprising,” he said. A severe course of any illness can lead to lingering effects.
Hviid and his colleagues aren’t the only researchers to find that long-lasting Covid-19 symptoms are rare for people with mild illness. A 2023 study looked at the electronic health records of a nationally representative sample of Israeli citizens with mild cases of Covid-19. It found that they were “at risk for a small number of health outcomes.” But most of the symptoms resolved within a year.
That study “confirms the statements that we’ve made that by and large, by one year, most people will have recovered,” said Theo Vos, an epidemiologist who helps track long Covid for the long-running Global Burden of Disease study.
Vos is an author of a 2022 systematic review that pooled data from 54 studies and two medical records databases, then grouped study participants into three symptom clusters: one centered around fatigue, another around cognition, and a third around breathing problems. The authors found that, among non-hospitalized people, just 0.7 percent had not recovered by 12 months after infection. This compared with 11 percent of those who were hospitalized and around 20 percent of those whose hospital stay involved the ICU.
In an April email, Selvakumar pointed out that many early long Covid studies were conducted on non-immune populations. That’s important to keep in mind, he wrote, because “the largest risk factor for long Covid is initial severity.” Thanks to immunity from vaccines and prior infection, most people today are less likely to have a severe course of the illness — thus, their risk of long Covid has declined as well.
Comparing an Al-Aly study of mental health outcomes with Hviid’s offers a glimpse into the dizzying number of variables that can influence a study’s results — even when, on the surface, the studies appear similar.
“There are huge differences” between the two studies, said Jeffrey Morris, director of the Biostatistics Division at the University of Pennsylvania’s Perelman School of Medicine. He started ticking them off: different study populations, different designs, different time periods.
Both approaches, Morris said, had merit.
Other researchers agreed that Al-Aly’s studies have merit, but stressed that the work is limited in its ability to speak to long Covid in the broader population. As a group, VA patients are older and less healthy. As a result, they are at higher risk of severe infection that might lead to hospitalization or even a stay in the ICU, events that increase one’s risk of long Covid. The VA studies look at “a very special group of high-risk people,” wrote Selvakumar in an email, “so you have to be very careful when extrapolating to the general population.” While a given study may note this limitation, he continued, the caveat sometimes gets lost in what he characterized as media spin.
One researcher doing similar studies was cautious about extrapolating his findings to the broader population. Junqing Xie, a post-doctoral researcher at the University of Oxford, recently co-authored a paper that used data from the U.K. Biobank to look for a connection between a Covid infection and psychiatric disorders and prescriptions. Similar to the VA team, Xie’s team found a link. However, it’s unclear what precisely this means for the general population, said Xie. “We are not able to infer any prevalences,” he told Undark. To do that, a researcher would need to ensure that their study participants are highly representative of the broader population. Neither the BioBank nor the VA databases meet this criterion, he said.
Within the already-less-healthy VA population, some experts said, Al-Aly’s infected groups probably skew toward more serious Covid-19 cases. That’s because people with asymptomatic or mild cases are much less likely to visit a doctor, who would then document the positive result in the patient’s electronic record. The effect would have become increasingly pronounced as time wore on and people developed immunity and started testing at home, said Makam. He pointed to a VA study that looked at the risk of organ damage associated with reinfection. People with multiple Covid infections documented in their health records probably had relatively more severe courses of illness, he said. This doesn’t mean that the average person who gets reinfected and can manage their illness at home is at heightened risk of organ damage.
(The study, published in Nature Medicine, doesn’t mention this as a limitation, though it does suggest that bias could run in the opposite direction: If people with Covid-19 don’t get tested, and if they are at heightened risk of bad outcomes, then they could make the uninfected group look sicker than it actually is.)
Some experts also raised concerns that the VA St. Louis team has worked with data in ways that, from the outside, don’t clearly map onto established statistical practices.
In his email, Lipsitch raised questions about the group’s use of negative controls, a statistical technique that can help a researcher determine whether any associations — for example, an association between a Covid-19 infection and smell loss — are causally linked.
In an influential 2010 paper, Lipsitch and his colleagues proposed that negative controls should be routinely deployed in epidemiological studies. Applied to the study of long Covid, one type of negative control, called a negative outcome control, might involve identifying health conditions that are highly unlikely to be caused by the infection: accidental injuries, for example, or scarring. If an infection were found to be associated with one or more of these unrelated conditions, then this would suggest that some other variable — something other than the Covid-19 infection — is influencing the study’s results.
In order for this technique to work, said Lipsitch, researchers need to define their negative outcome controls before they conduct their analysis, and then report all the findings. The VA St. Louis’ first paper used neoplasms — a medical term for tumor — as a negative outcome control, but in the preprint, neoplasms were not treated as a negative control; rather, they were treated as an ordinary outcome. “There are also issues about how the negative outcome controls were chosen in subsequent papers,” Lipsitch wrote to Undark. The negative outcome controls differ across studies, he said, and it’s not clear why.
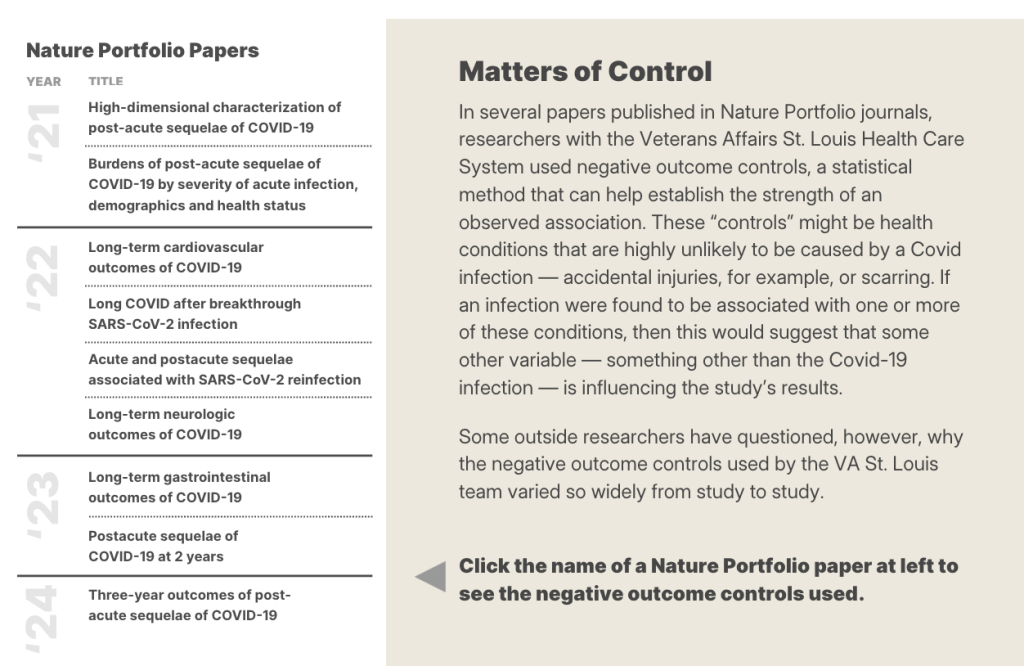
Some of this is difficult to parse, Lipsitch said, because the study’s methods are not clearly explained. “I think this is a case where peer review didn’t do its full job,” he said. “Because part of what peer review should do is to ensure that people with expertise in the field, ideally can reproduce, but at least can understand — in detail — what was done and make a judgment of how valid it was. And in this case, in its wisdom, Nature decided to let through a series of papers that describe their methods in such vague terms that it’s really hard to know what was done.”
Hviid also noted that the VA team changes its negative controls, along with its comparison groups, from study to study. “It’s a little bit weird,” said Hviid. Ideally, a research team would establish its analytical setup and then, whenever it wanted to add more data, the team would rerun the analysis using the same design. “I’m not saying that they’re intentionally fraudulent,” Hviid added, “but you’ve really got to be careful as a researcher if you’re sitting and running a lot of different analyses.”
The VA St. Louis team also used different approaches — including different weighting methods and a regression adjustment — to make its Covid and non-Covid groups comparable.
There might have been valid reasons for a research team to make such changes, experts told Undark. Peer reviewers might have requested them, for example. When asked about this by email, however, Al-Aly did not provide a rationale.
Undark also shared many of these concerns in a detailed email to Nature, whose portfolio journals published nine of the VA St. Louis’ long Covid studies. In response, Isobel Lisowski, a communications officer for Springer Nature Group, forwarded a statement on behalf of Nature Portfolio, which she asked to be attributed to Magdalena Skipper, editor-in-chief of Nature: “Our journals are editorially independent of each other, and each paper is assessed and peer reviewed independently based on its own individual merits. At all times our commitment is to ensure the accuracy of the scientific record and, if concerns are raised with us directly, we look into them carefully.”
The statement further noted that the VA St. Louis papers used several approaches to test the robustness of the findings, and that a reporting summary was published with each paper to increase transparency.
The BMJ, which published the VA St. Louis’ paper on mental health outcomes, published notes from the peer review. The reviewers did not raise the topic of negative controls. The VA St. Louis team did indicate that it was building additional cohorts to address reviewers’ concerns about possible bias in the study design.
Al-Aly is not unaware of the criticism. “I love these questions,” he said, wrapping up the first interview with Undark, during which he discussed his research as well as its possible limitations.
In conversation, Al-Aly is warm and funny, peppering his sentences with colorful idioms and playful hyperbole. (“You could test your cat if you wanted to. You can test your dog,” he said, recalling how Americans initially went all-in on at-home Covid testing.) He’s also willing to brawl, at times suggesting that many of his critics lack the expertise to evaluate his work or produce good research of their own. “We get a lot these newbies. They want to do studies,” he said. But their work sometimes contains what he characterized as “sophomoric mistakes.”
One example, in his view: the 2023 Israeli study of people with mild symptoms, which was published in the BMJ. “Do me a favor and look at their Figure 7,” said Al-Aly, off the top of his head, when asked about the paper.
Al-Aly pulled up the study on screen. Figure 7 shows that the vaccinated individuals in the study were at a higher risk for memory problems than the unvaccinated. The most plausible explanation, said Al-Aly, is that the researchers haven’t fully accounted for bias in their dataset. Further, he said, the study seems to assume that if a diagnostic code stops appearing in a patient’s medical record, this means the condition has resolved. In reality, said Al-Aly, “it’s very hard to document the resolution of symptoms in EHR.”
(In an email to Undark, a study co-author, Maytal Bivas-Benita, said that the memory finding wasn’t statistically significant. She added that her group’s findings are supported by a more recent Israeli study, which found a return to baseline in medication use and health care costs in non-hospitalized Covid-19 patients.)
Al-Aly was also critical of the study from Hviid’s team. Their control group, he suggested, consists of people who tested negative. The distinction matters because during the pandemic people with worse baseline health tended to test more frequently. A cancer patient needing chemotherapy in 2020, for example, would first need a negative Covid test. “When you compare sick people to sick people, you’re not going to find big differences,” said Al-Aly.
Speaking about the Danish study, Al-Aly said, “it’s not unreasonable to even call it deeply or fundamentally flawed.”
(“Clearly he has not read the paper very carefully,” said Hviid. His team’s control group included everyone without a positive test. While they did perform an additional analysis with a test-negative control group, Hviid said, it yielded the same results. )
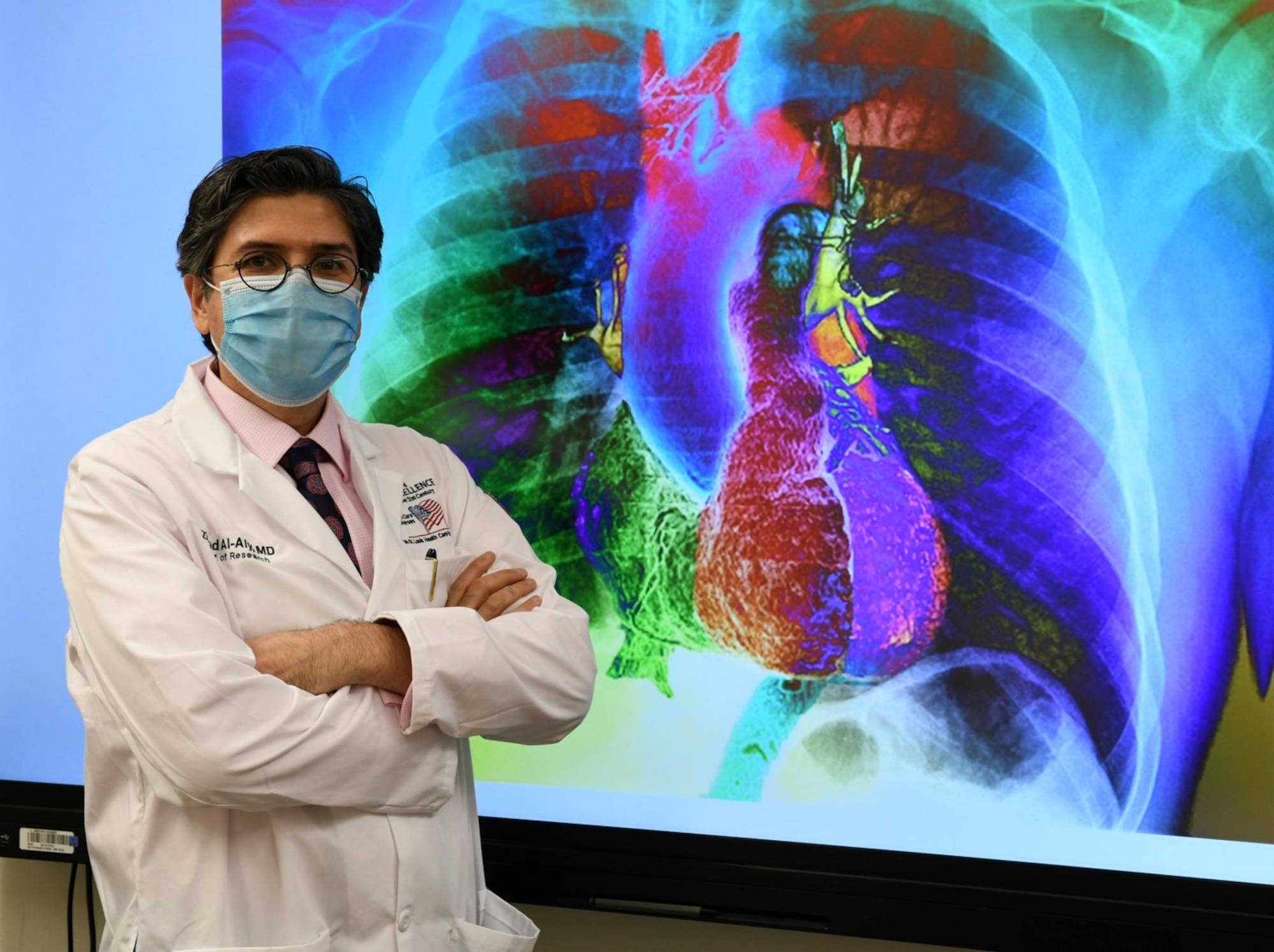
Ziyad Al-Aly, who holds positions at Washington University in St. Louis and at the Veterans Affairs St. Louis Health Care System, is not unaware of the criticism surrounding his research. He’s also willing to brawl, at times suggesting that many of his critics lack the expertise to evaluate his work or produce good research of their own. Visual: Mary-Dale Amison/VA
According to Al-Aly, VA samples can speak to the broader population. While it’s true that VA demographics don’t perfectly mirror the rest of the U.S., it’s reductionist to dismiss the findings on these grounds, he said. The average age of VA patients is about 60, but this figure represents a large distribution, said Al-Aly. And while women are about 10 percent of the VA’s population, this can translate to more than 600,000 people in a VA study. “We can fill 10 — 10! — Taylor Swift stadiums” with women, he said, which makes it possible to look for sex differences in their findings.
He also said they adjusted for differences in testing and access to testing over time. This would substantially reduce any bias if it existed, said Al-Aly. (The VA team adjusted for “a huge list of confounders,” said Morris, when commenting on the study of neurological and psychiatric outcomes.) “But having said that,” said Al-Aly, now speaking specifically about his group’s reinfection study, “it’s not unreasonable also to interpret the study, ‘these are the results, and the results really reflect the people who actually tested.’”
Nonetheless, Al-Aly said, knowledge from VA studies can be applied to the general population.
Speaking with Undark, Eric Topol pointed to a May Substack post that he co-authored with Al-Aly. It highlighted a number of studies that he described as aligning with the VA research. One was an EHR-based study from Italy, which found that people infected with Covid-19 had elevated rates of cardiovascular problems even three years after infection. (The study did not distinguish between Covid-19 patients who were hospitalized vs. not hospitalized.) The post also described a longitudinal study of patients who were hospitalized with Covid-19 in Wuhan, China. Three years after their initial infection, more than half reported at least one symptom, most of which were mild to moderate.
Long Covid, said Topol, is “prevalent. It doesn’t go away normally. There are some people that are lucky that they fully recover, but most kind of limp along.”
Like Topol, Al-Aly also said that long Covid recovery is rare, particularly among people who have significant post-exertional malaise or fatigue that lasts more than several months. Clinicians are not seeing recovery in these patients, he said.
Although Al-Aly was one of many co-authors on the Global Burden of Disease’s systematic review that found most people do recover, he said that the findings need to be interpreted with caution. The review’s primary goal was to track symptoms, not recovery; and even then, the study did not track all long Covid symptoms. Additionally, the review drew from a wide variety of studies — some based on surveys, others on clinical assessments, and yet others on information in databases. This is not the best way to assess recovery, he said, because long Covid symptoms sometimes come and go. A person may have brain fog that lets up for a while, only to return later. The best way to assess for recovery, said Al-Aly, is to follow people over time, checking in every three months or so.
(“That is an interesting point of view,” Vos wrote after Undark shared some of these concerns with him. “I think we had enough studies in our 2022 paper to reject the hypothesis of no recovery.” He added that his research team is currently working on an updated analysis: “It does look like there will be a small subset of people who remain symptomatic years after infection.”)
Later, when asked by email about specific critiques involving negative controls, Al-Aly described them as “grossly unfair.”
In response to a separate email asking about the different statistical approaches used to make his Covid and non-Covid groups comparable, Al-Aly pointed back to the Israeli study, the Danish study, and the Global Burden of Disease study: “We are criticized for using negative controls,” he wrote. These other studies “don’t use any means of quality control. Quite ridiculous that you criticize us for doing the right thing and elevating the rigor of the work.”
The scientific debate over long Covid has unfolded amid undeniable human suffering. Across the country, clinics have reported handling an influx of cases since 2020. Previously healthy individuals may suddenly find they need to sleep 18 hours a day. They may struggle with brain fog and breathlessness. Many people have had to scale back on work or quit their jobs entirely. Specialized care is often difficult to access, particularly for Black and Latino patients.
A post-viral condition can steal your whole life, a patient advocate told Undark. In severe, or even moderate cases, “you’re stuck in bed all day, you lose your friends, you lose a lot of your family, you lose your jobs, you lose your aspirations for life. If you wanted to have kids, if you wanted to get into a relationship, if you wanted to start a business, if you wanted to continue a hobby — all of that is gone.
“You’re just kind of suspended in life and dependent on the outside world to come to your rescue,” the patient advocate continued.
Those patients often find themselves facing skepticism from people who do not believe the condition is real — including, in some cases, their own doctors. And they are navigating symptoms at a time of intense political polarization over the implications of Covid-19.
The idea that long Covid is widespread, and that its numbers are growing, can be comforting for long Covid sufferers, said the patient advocate, who spoke on condition of anonymity in order to avoid blowback from within the patient community, which the advocate said, views Al-Aly as a god-like figure.
“He is beloved by patients. And I’ll tell you why I think he’s beloved by patients: because patients feel left to rot and die, and he has told them what I think some people interpret as a scary story, which is ‘long Covid is rampant. Everyone’s going to get long Covid. It’s going to disable the population,’” the advocate said. “To a patient, this is not a scary story. To a patient, this is actually a very hopeful story because everyone’s going to get sick; they’re going to have to help me.”
But the advocate expressed deep misgivings about promoting exaggerated views of the number of people at risk of developing long Covid. Such views won’t “help to have you taken seriously by skeptical people.”
For now, U.S. public health authorities — drawing on the research of Al-Aly and his colleagues — have continued to trend toward the broadest possible definition of long Covid.
The recent National Academies of Sciences, Engineering, and Medicine report recommended a new definition of long Covid for the U.S. government and health care system. The final result looks remarkably similar to Al-Aly’s description of the disease: Long Covid can be mild to severe, the report states, and it may include just one symptom or a single new diagnosis that develops after a SARS-CoV-2 infection and persists for at least three months.
In practice, this means that if a person has a mild case of Covid — say a cough and fatigue lasting one week — and then develops a chronic condition like lupus six weeks later, this new lupus patient could also be diagnosed with long Covid. “Clinicians must exercise their judgment and rely on evidence in reaching a diagnosis in any individual patient,” wrote Harvey Fineberg, a prominent public health expert and chair of the report, in an email to Undark.
Fineberg pointed to electronic health record data suggesting a large jump in rates of lupus onset after a Covid-19 case. Given that, he wrote, “a clinician would be wrong some of the time, but they would be more often wrong if [they] failed to ascribe the condition to long Covid.”
The long Covid diagnosis, Fineberg added, could help patients understand where the lupus came from, and perhaps in the future suggest treatments.
Public health expert Harvey Fineberg chaired a recent report which offered a new definition of long Covid. Fineberg stressed that “clinicians must exercise their judgment” in reaching a diagnosis.
Visual: Christopher Michel/Wikimedia Commons
But Putman, the Wisconsin rheumatologist, who treats lupus patients, noted that not all studies have found such a strong connection between an infection and lupus. He pointed to 2023 paper that actually found a protective effect of Covid-19 against lupus. “Do I believe that? No,” he wrote in an email. The real issue is “the data in this area are all very uncertain and often contradictory.” It’s implausible, he added, that the majority of new lupus diagnoses have been driven by Covid-19 infections. If this were the case, “we would expect a dramatic increase in the yearly rate of new lupus diagnoses. As far as I can tell, the incidence is more or less stable.”
Putman added that it would be difficult to run an effective clinical trial using a broad definition. The study participants would likely have multiple underlying pathologies, he said, that don’t all respond to the same treatment.
This new definition may also undermine the real and profound suffering experienced by some people with post-viral illness, said Leonard Jason, a psychology professor at DePaul University who has long studied ME/CFS, a severe condition marked by life-altering fatigue. “If a person has trivial pain in the toe for 3 months following Covid infection, with no negative consequences to the person’s functioning or quality of life, that person would still be eligible for a long Covid diagnosis,” he wrote in a recent opinion piece for Medpage Today. It’s a mistake to ignore symptom frequency and severity, he wrote.
The report recommended that the definition should be reviewed and possibly updated in no more than three years’ time, as the science continues to evolve.
“During the pandemic, the quality of research went down,” said Anders Hviid during a May Zoom call. “I think some scientists and probably also journal editors became a little one-sided or blind. Maybe it was because it became so polarized. So, people were either in one camp or the other.” There’s no question, he continued, that harmful symptoms can follow Covid-19 infections. But conversations about the frequency of those symptoms seemed out of touch, he suggested, particularly as time passed and the risk of developing long Covid declined as people acquired immunity.
Makam, in San Francisco, meanwhile, has spent years studying long-term health outcomes of people with prolonged serious illnesses. He worries about the consequences of having a poor case definition for long Covid. “How can you study a disease if you’re defining your illness very, very broadly, including a lot of different pathologies into this one disease syndrome?” He was blunt in his assessment of the work coming out of the VA St. Louis. “We’re going to look back and that entire line of work is going to be wrong. Like very wrong.”
Al-Aly’s third interview with Undark took place on May 30, the day Nature Medicine published his three-year follow-up study of patients with a documented Covid-19 infection in 2020. He had been up late the night before, putting together a thread on X, the platform formerly known as Twitter, with key points. It wasn’t all bad news, he wrote. Over time, people in the infected group became significantly less likely to die or develop new onset disease. Yet even three years out, those with mild infections remained at increased risk for some new onset symptoms.
He also expressed frustration with some of the criticism that has come his way, particularly on social media. “Good scientific criticism can sharpen the focus of the inquiry and make it better,” he said. But all too often, the critiques don’t serve any clear function and may even feed into denialism. “A lot of people feel sick and tired of this pandemic and want to move on, which is totally, totally understandable. Like, who doesn’t understand that? Who doesn’t sympathize with that?” Still, he said, the fact remains that many people need help, and he plans to help them — his detractors be damned.
“To the chagrin of the critics, we’re going to keep moving the ball forward,” Al-Aly said. If that irritates people, they’ll just have to get used to it, he added. “We’re working day and night to solve this problem.”