By Alex Hollingsworth, Associate Professor at The Ohio State University, Krzysztof Karbownik, Assistant Professor, Department of Economics at Emory University, Melissa A. Thomasson, Professor of Economics at Miami University, and Anthony Wray, and Associate Professor at University Of Southern Denmark. Originally published at VoxEU.
Both Black and white infant mortality rates in the US have fallen in the past century, but racial inequality in infant mortality is worse. This column studies the impact of a large-scale hospital modernisation programme in the 20th century on healthcare capacity and mortality outcomes, with a focus on racial inequality. Upgrading healthcare reduced infant mortality rates and narrowed the Black-white infant mortality gap by one-quarter. The cost-effective investments in healthcare infrastructure disproportionately benefited historically marginalised groups, had long-run benefits, and complemented, rather than substituted, medical innovation.
Article 25 of the Universal Declaration of Human Rights states that “[e]veryone has the right to a standard of living adequate for the health and well-being of himself and of his family, including … medical care and necessary social services” (United Nations 1948). Despite this, much of the world’s population lacks access to physician and hospital care. In 2017, North America had 2.7 hospital beds per 1,000 people, while South Asia had only 0.6 (WHO 2017).
Access also varies within high-income countries. The US and Switzerland have the largest per capita health expenditures in the world, but the US has 60% the hospital beds and doctors per 1,000 people when compared to Switzerland (Papanicolas et al. 2018, WHO 2020). The COVID-19 pandemic (Propper and Kunz 2020) along with trends in healthcare centralisation, physician shortages, and insufficient funding, could further limit access, creating health deserts, especially in socioeconomically and racially disadvantaged areas. Research on the impact of reducing hospital capacity is mixed. Kozhimannil et al. (2018), Germack et al. (2019), and Gujral (2020) report adverse effects of hospital closures, while Fischer et al. (2024) do not find the same results.
In the US, these challenges persist despite dramatic changes in healthcare spending and population health over the last century (Cutler et al. 2019). In the last century, healthcare spending has increased tenfold, infant mortality has declined 95%, and life expectancy has risen by 45% (Costa 2015). However, these impressive gains have not been equal across racial groups (Muller et al. 2019). In 1916, the infant mortality rate per 1,000 live births was 184.9 for Black infants and 99.0 for White infants, yielding a ratio of 1.9 (Singh and Yu 2019). By 2021, Black and White infant mortality rates had fallen to 10.6 and 4.4, respectively, but the gap had widened to a ratio of 2.4 (Ely and Driscoll 2023). Thus, despite the massive overall declines, racial inequality in infant mortality is worse now than it was at the beginning of the 20th century.
Given these two realities – unequal access to healthcare and racial inequality in health outcomes – it is imperative to understand if investments in healthcare infrastructure can reduce these deficiencies, especially since healthcare now plays a central role in contemporary society, accounting for nearly 20% of the US economic activity.
The Duke Endowment modernisation campaign and its effects on the hospital sector
In a new paper (Hollingsworth et al. 2024), we study how funding for healthcare infrastructure affects healthcare capacity and mortality outcomes, with a particular focus on racial inequality. Our work is based on a unique quasi-experiment: a large-scale hospital modernisation programme supported by the Duke Endowment in North Carolina during the first half of the 20th century. The charity assisted hospitals in expanding and improving existing facilities, obtaining state-of-the-art medical technology, and elevating their management practices. In select communities, it also helped to build new hospitals or to convert existing facilities to non-profits. Although the funding only started in 1927, by the end of 1942 the Endowment had appropriated over $53 million (in 2017 dollars) to the state.
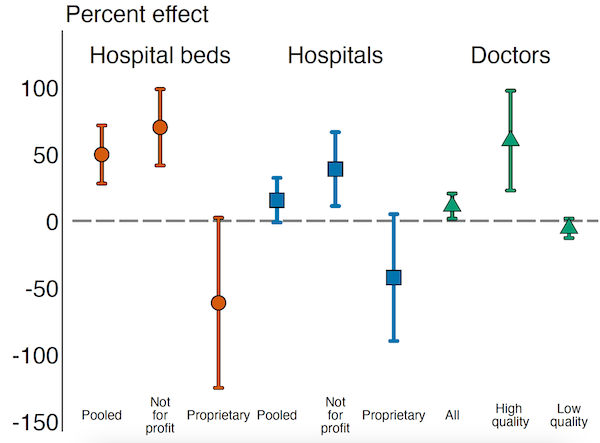
The funding increased the number of not-for-profit hospitals per 1,000 births that were eligible for funding, while causing a decline in ineligible for-profit hospitals (Figure 1). This substitution effect was mirrored in hospital beds: not-for-profit beds increased by 70.1% while for-profit beds declined by 61.4%. This led to overall increases in both institutions and beds. Furthermore, supported communities saw a 60.2% increase in high-quality physicians per 1,000 births and a 5.5% decrease in poorly trained physicians, advancing the average state of medical knowledge in Endowment supported locations (Figure 1). These effects persisted for more than 30 years, suggesting a lasting increase in capacity.
Figure 1
Effects on Infant and Long-Run Mortality
Changes in healthcare infrastructure help explain our core finding that Duke financial support improved health outcomes in these communities, causing a 7.5% reduction in the infant mortality rate (Figure 2). The gains were about three times larger for Black infants (13.6%) compared to White infants (4.7%), narrowing the Black-White infant mortality gap by one-quarter. Furthermore, those exposed to the support around the time of birth also enjoyed lasting health effects, with long-run mortality rates (between the ages 56 and 64) declining by 9.0% – a benefit that accrued similarly for both races. These investments were cost-effective. One life was saved for every $17,092 (in 2017 dollars) paid to hospitals, a cost significantly lower than any reasonable estimate for the value of statistical life.
Figure 2
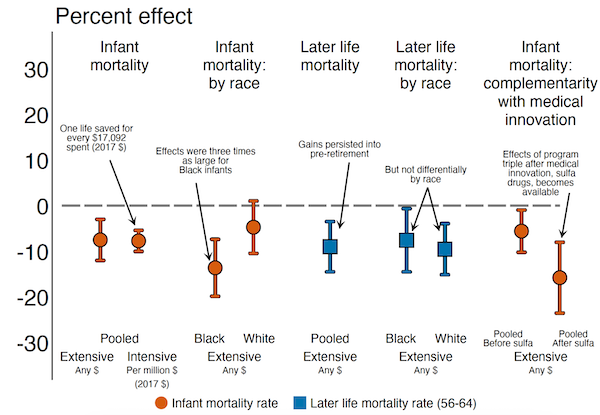
Complementarity Between Capital Investments and Medical Innovation
Finally, we document that Duke-supported hospitals used new medical advancements more effectively, suggesting a complementarity between high-quality hospitals and new medical interventions (Figure 2). We explore this by estimating the interaction between Duke support and the 1937 discovery of sulfa drugs, which effectively treated pneumonia. We observe no effects of Duke funding in locations with low baseline pneumonia mortality. On the other hand, in places with high baseline pneumonia mortality, the gains are present both before and after the medical discovery, but the effects are almost three times larger in the post-antibiotic era. This reflects the complementary nature of hospital modernisation with medical innovation, which in this case may be explained by the fact that the Endowment attracted more-qualified physicians to the area who were better able to leverage the new technology.
Conclusions
We conclude that investments in healthcare infrastructure: (1) lead to permanent improvements in the supply and quality of healthcare available to the affected residents; (2) provide short- and long-run mortality benefits; (3) disproportionately benefit historically marginalised groups; (4) complement rather than substitute medical innovation; and (5) are cost-effective – at least in a setting where initial levels of healthcare supply are low, as is still the case in many low-income countries today.