Yves here. KLG compares the performance of the medical and scientific establishment in two pandemics: HIV and COVID-19. He systematically works his way to the conclusion that a vaccine-dominated approach when there has been no example of a durable success in preventing infection or contagion for a coronavirus, amounts to scientific malpractice.
KLG’s intro:
Two pandemics forty years apart illustrate how politics, society, and science converge during a worldwide medical emergency. The response to HIV/AIDS occurred in a different world, in which biomedical science was not yet an adjunct of Big Pharma and Big Medicine. AIDS is still with us, but we have the knowledge if not the political acumen to treat it if not vanquish it. COVID-19 emerged long after the neoliberalization of science had taken hold, and our progress in dealing with another worldwide pandemic seems to have generated more heat than light, although AIDS generated some of the former. Different assumptions, different politics, and different infrastructures determined the response to COVID-19, and we are still dealing with a great deal of uncertainty regarding the origin and likely progression of COVID-19, whatever the politico-medical establishment would have us believe.
By KLG, who has held research and academic positions in three US medical schools since 1995 and is currently Professor of Biochemistry and Associate Dean. He has performed and directed research on protein structure, function, and evolution; cell adhesion and motility; the mechanism of viral fusion proteins; and assembly of the vertebrate heart. He has served on national review panels of both public and private funding agencies, and his research and that of his students has been funded by the American Heart Association, American Cancer Society, and National Institutes of Health.
I was an eager researcher at the beginning of the HIV/AIDS pandemic, when every issue of Science, Nature, and Cellfrom 1982 to1988 and beyond contained the latest scientific results on this horrible affliction that amounted to a death sentence. This was an exciting but even scarier time, and so far AIDS has killed 42 million people since 1981. COVID-19 came along forty years later when I was much older and considerably more experienced in the practice of biomedical research, inside and outside of the laboratory. These past five years have also been exciting, but less for the science than for the politics. The exact death toll from COVID-19 cannot be known with precision but according to Our World in Data, 27 million people are estimated to have died above previous death rates in the past five years.
What follows is an essay in the original sense of essai from the French, an attempt to understand a critical current issue. I have used Chapter 7 of Choose Your Medicine: Freedom of Therapeutic Choice in America (Lewis A. Grossman, Oxford, 2002) as the framework I had been seeking to address this topic. This book was discussed in my previous post on Politics and Medicine. The similarities between the AIDS and COVID-19 pandemics lie in one question: What do you do in a medical emergency that transcends the practice of medicine and extends deeply into society, culturally and politically, as well as scientifically and geographically?
When AIDS appeared, intractable infectious diseases were thought to be a thing of the past. Smallpox had been eradicated. Tuberculosis, also called consumption, was still present but the “White Death” that killed millions through the nineteenth century [1] and well into the twentieth century had receded. Polio vaccines had removed the overwhelming fear of polio even though cases continue to appear where the vaccine is not universal. Alarms about the misuse of antibiotics and the emergence antibiotic-resistant bacteria could be heard in the background by those listening, going back to Sir Alexander Fleming’s comment while visiting the United States after World War II that indiscriminate use of antibiotics, including the miracle drug penicillin he discovered, in young children as a prophylactic against bacterial disease could not be a good thing. AIDS showed that our complacency was misplaced.
In June 1981 five cases of an odd, probably infectious, disease were reported. [2] An article about GRID (Gay Related Immune Deficiency) appeared in The New York Times in 1982. The title of the article – “New Homosexual Disorder Worries Health Officials” – explains much of the subsequent politics of HIV/AIDS. This was covered exceedingly well by the late Randy Shilts in his book And the Band Played On and in the HBO film that follows the book faithfully. At that time of the NYT article, 335 people had been diagnosed with GRID and 136 had died, a mortality rate of 41% that eventually approached 100% in that cohort, a grim presentiment.
The mode of HIV transmission through exchange of bodily fluids (sex, transfusion, intravenous drug abuse, needle stick in a clinical setting) was identified quickly. Non-pharmaceutical interventions (NPI) to prevent transmission of HIV soon followed. These included the use of physical barriers (condoms), changes in behavior, and testing the blood supply for HIV as soon as the necessary reagents became available.
From the beginning of the epidemic, research on AIDS was both frantic and productive, while using techniques that were primitive by current standards. [3] In 1983, Human Immunodeficiency Virus was described in back-to-back papers by Luc Montagnier and Françoise Barré-Sinoussi of the Pasteur Institute and Robert Gallo at the National Cancer Institute (NIH) in Science. As noted above, epidemiologists and Infectious Disease physicians had by then determined how to stop transmission of HIV, provided their recommendations were followed. Molecular biologists, virologists, biochemists, immunologists, and cell biologists elucidated the HIV life cycle and how the virus damages the immune system and prepares the way for the varied opportunistic infectious diseases and cancers that kill AIDS patients
Scientific politics also affected research on HIV/AIDS, and Grossman covers this well in Choose Your Medicine(eBook). In the early days of AIDS, virtually nothing worked as a pharmaceutical intervention. AZT was made available on a compassionate basis, but it was not effective in many, perhaps most, patients and the side effects were often severe. Activists rightly wanted something that did work and were willing to try anything with promise. At the time, however, the Federal Drug Administration (FDA) was slow to act in the eyes of the affected community. And this was not necessarily the wrong stance given the history of drugs gone awry, such as thalidomide and diethylstilbestrol. The primary focus of scientists and administrators at FDA was to “prevent harm to consumers [4] rather than facilitate the introduction of useful new products” (Grossman, p. 169). Preapproval access to drugs was rare in the absence of a full 3-phase clinical trial testing safety, effectiveness and side effects, and effectiveness and adverse reactions.
Dr. Anthony Fauci was named Director of the National Institute for Allergy and Infectious Diseases (NIAID) in 1984. He and most of his colleagues were reluctant to approve potential drugs for AIDS in the absence of complete evidence for their safety and effectiveness. But he soon allowed the AIDS activist community into the decision-making process and what has become known as the parallel track for development and evaluation of novel drugs was initiated. Basically, in the parallel track, unapproved but promising drugs would be made available as soon as they were shown to be safe while the larger trial was still ongoing. Fauci did this by going around the FDA, not without some push back. His was correct.
The results were equivocal in the short term, but the parallel track was the correct path to take in such a dire emergency. The FDA ruled in 1992 that a new drug could be approved if adequate, controlled studies established that the drug led to a clinical endpoint indicating a reasonable likelihood for a positive clinical benefit. This is conditional but valid scientific and clinical approach. In the event, early trials of HIV/AIDS multidrug therapy (HAART) showed that CD4 cell counts increased in patients taking these drugs in combination. This indicated recovery of the immune response that had been destroyed by HIV. The treatment regime was onerous – many pills on a strict schedule – but promising. Multidrug therapy subsequently succeeded in reducing the death rate from AIDS in the US from a frightening peak of ~50,000 in 1995 to less than 20,000 in 1997 (still frightening but a remarkable decrease in deaths).
The result was that AIDS became a manageable condition for most of those with HIV who are treated with HAART – Highly Active Anti-Retroviral Therapy – an approach that attacks HIV at three or more levels, including viral RNA replication, integration of the HIV genome into host cell DNA (responsible for the persistence of HIV), and proteolytic processing of viral proteins essential for HIV assembly and maturation into infectious virus. NPIs also still work and Pre-Exposure Prophylaxis (PrEP) has recently become available for those at risk of HIV infection, but not without a fair amount of medical political economy involved. [5]
On the other hand, an HIV vaccine has been “in the works” since the early-1980s. Every few years an advance appears on the horizon. A recent news article in Nature (paywall) summarizes current prospects:
The field has made steady progress towards a vaccine since the first HIV infection was reported in 1981 — but there’s still a long way to go…One of the biggest challenges…is developing a vaccine that can broadly neutralize the multiple strains of HIV. The virus is also…In a pair of papers published in Science Immunology…researchers report an immunogen that can generate potent, broadly neutralizing antibodies against HIV in macaques…making it…possible to at least begin the process of engaging immune cells to produce broadly neutralizing antibodies. The immunogen, dubbed GT1.1, is currently being tested in a phase I clinical trial. (emphases added)
After all these years a promising HIV vaccine remains stuck at Phase 1, but the preliminary data are promising once again.
During the early days of HIV/AIDS the FDA and the scientific establishment represented by NIH were viewed as slow to act. But focused research on HIV led to interventions that prevented transmission of HIV. These NPIs and changes in behavior were critical in the early stages of the HIV/AIDS epidemic. They remain so after nearly 44 years. And all of this played out under what Lewis A. Grossman has called America’s Drug Constitution that includes, especially, bodily freedom, economic freedom, and freedom of inquiry:
- The patient has the right to therapeutic choice, and in the case of HIV/AIDS this was mostly done within the boundaries of conventional medicine rather than alternative medicine, despite conflicts between patients and the medical establishment.
- The patient and patient advocates have the right and obligation to question the authority of the medical establishment.
- Throughout the HIV/AIDS pandemic freedom of scientific inquiry remained an overarching criterion for research on AIDS.
Compared to the early days of HIV/AIDS, it seems at this remove that reactions by the political and medical establishments were faster when SARS-CoV-2 emerged in Wuhan five years ago. These reactions also seem to have been qualitatively different in both approach and in relation to the implicit Drug Constitution. Aside from a few outrageous hypotheses [6], AIDS was recognized immediately as an infectious disease transmitted by the exchange of bodily fluids. Transmission by casual contact with AIDS patients, airborne transmission, and mosquito bites were ruled out early.
Identification of HIV as the agent of AIDS took two years of painstaking experimental work in different virology laboratories. SARS-CoV-2 was identified as the cause of COVID-19 on a timescale that can be measured in days, because SARS and MERS had come before and sophisticated experimental and analytical techniques were available. The original SARS/SARS-CoV-1 spread fairly easily but the outbreak subsided quickly. MERS had a much higher death rate but was not as transmissible as SARS. That SARS-CoV-2 is airborne was slow to catch on, perhaps because of previous experience with SARS and MERS. Nevertheless, SARS-CoV-2 is an airborne virus, and there can be little doubt that wide recognition of this fact before COVID-19 became pandemic would have slowed the spread of the disease through the use of NPIs (e.g., social distancing, N95 masks, and air filtration).
Vaccination as the one preferred approach to COVID-19 dominated the first years of the pandemic. Several vaccines remain under investigation but the mRNA vaccines from Pfizer and Moderna dominated the field in the beginning There is nothing experimental about these vaccines, in that development and production required nothing outside standard modern molecular biology. But, more importantly, there was virtually no research indicating vaccines against SARS-CoV-2 will work. An mRNA vaccine for Zika virus has yet to pass clinical trials and development subsequently slowed after the initial Zika outbreak in the Americas.
But more importantly, the first coronavirus was identified ninety (90) years ago as Infectious Bronchitis Virus (IBV; identification of its “corona” had to wait until after WWII for the electron microscope). As noted in the abstract to the paper at the link:
>(D)espite decades of extensive immunoprophylaxis efforts, IBV remains a major health concern to poultry producers worldwide. Rapid evolution due to large poultry population sizes coupled with high mutation and recombination events and the reliance of the antiviral immune response on specific antibodies against the epitopes of the S1 glycoprotein, render the control of IBV extremely challenging. (emphasis added here and below)
There is no good reason to assume the mechanism of immune evasion in rapidly evolving RNA viruses in birds would be significantly different in humans. For example:
The emergence of SARS stunned medical scientists, but veterinary virologists had previously recognized CoVs as causing fatal respiratory or enteric disease in animals with interspecies transmission and wildlife reservoirs…Unfortunately, despite long-term efforts, effective vaccines to prevent enteric CoV infections remain elusive…Confirmation of the pathogenesis of SARS in humans or animal models that mimic SARS may further aid in vaccine design and evaluation.
And:
The current pandemic of COVID-19 has set off an urgent search for an effective vaccine. This search may well benefit from the experiences of the animal health profession in the development and use of coronavirus vaccines in domestic animal species. These animal vaccines will in no way protect humans against COVID-19 but knowledge of the difficulties encountered in vaccinating animals may help avoid or minimize similar problems arising in humans…Other issues that have been encountered in developing these animal vaccines include a relatively short duration of protective immunity, and a lack of effectiveness of inactivated vaccines. On the other hand, they have been relatively cheap to make and lend themselves to mass vaccination procedures (in CAFO [7] chickens and turkeys).
So, given that durable immunity against coronaviruses, through previous infection or vaccination, has been problematic since before WWII, it seems odd that Operation Warp Speed was the one path to stopping the pandemic. One might think this would render the Great Barrington Declaration (GBD), which was sponsored by the libertarian American Institute for Economic Research, somewhat suspect. Jay Bhattacharya, MD, an author of the GBD is in line to become Director of the National Institutes of health in 2025.
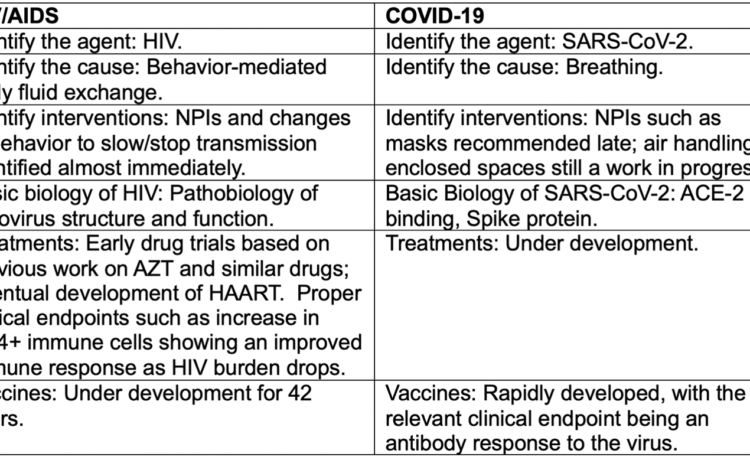
The mRNA vaccines were a tour de force of modern Biomedicine. By some suggested measures (e.g., moderating the course of disease in some patients) the Pfizer and Moderna vaccines were a success. Nevertheless, they do not stop transmission of the virus or prevent disease, which are the two functions universally expected of modern vaccines against life-threatening disease. A schematic side-by-side attempt at comparison between the responses to HIV/AIDS and COVID-19 may be useful:
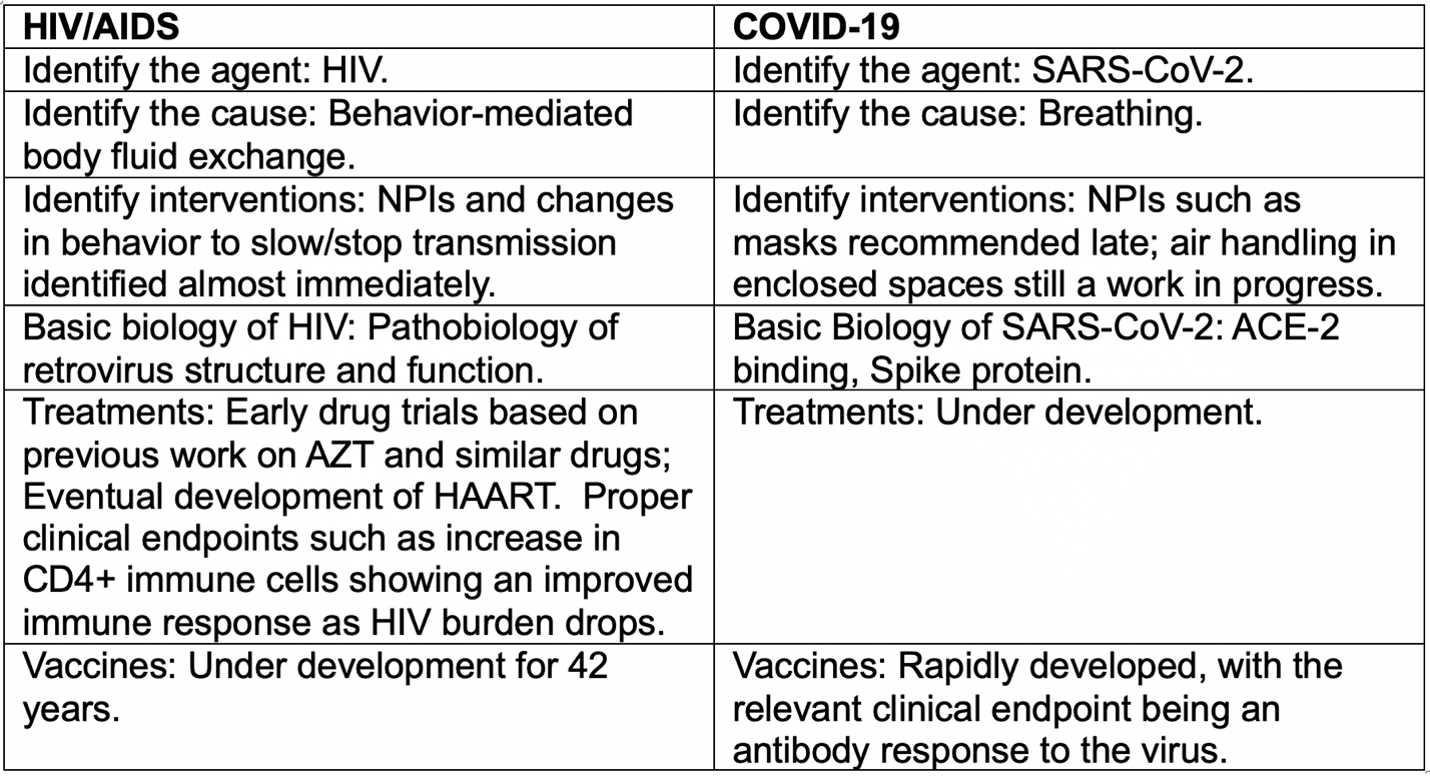
In no way is this meant to conflate two very different viral diseases. Rather the attempt is to compare the responses of the medical establishment to distinct though similar medical emergencies, forty years apart. Politics was involved in both. With HIV/AIDS this was unfortunately conventional and need not be relitigated. Suffice it say that until Rock Hudson admitted he had AIDS and appeared on TV with his costar Doris Day, the political establishment had ignored the epidemic.
The scientific politics of HIV/AIDS was fraught at the beginning, but Anthony Fauci and others led the way with the parallel track, which is now valid for all emergent diseases. In hindsight, it is difficult to see how the trajectory of HIV/AIDS research could have been fundamentally altered for the better. The origin and evolution of HIV and its pathobiology are well understood. HAART was the result. The costs and lack of availability of HAART and PrEP throughout the world remain a seemingly intractable political problem in need of solution, but the scientific foundations are solid.
Since COVID-19 is still in its early stages, judgment is necessarily tenuous. Although pharmaceutical treatments are under development for COVID-19, there have been few breakthroughs, yet. But the development of multidrug therapy for SARS-CoV-2 should be feasible, using the development of HAART as a broad outline. The nodes at which virus entry, replication, and assembly into infectious virions are well understood for coronaviruses. Intranasal vaccines in particular may prevent infection. Available tools are better forty years later, including rational drug design using algorithmic intelligence in some form.
What is puzzling from a scientific perspective is the initial emphasis on vaccines as the one best hope for curtailing COVID-19. If the FDA and CDC were slow to act early in the AIDS epidemic, they seem to have acted heedlessly during COVID-19. As noted above, scientific evidence on the futility of vaccines against animal coronaviruses is strong. Humans are social animals not so different from birds in CAFOs in many social situations. The apparent lack of appreciation of this fact is scientific malpractice in my view. This does not imply that vaccination will not eventually prevent coronavirus disease and transmission, but such an outcome seems unlikely based on current knowledge that is almost a hundred years old.
The novelty of the mRNA platform was undoubtedly responsible for much of the initial enthusiasm for these vaccines. The basic science is sound, but unproven. The critical early clinical endpoints were antibody response as a proxy for immune protection. However, clinicians, immunologists, and molecular cell biologists know that a measurable antibody response guarantees nothing about a functional antibody response in the experiment, the target cell, or immunity in the target organism.
It also seems clear the implicit Drug Constitution described by Professor Grossman has been left in tatters by the politico-medical response to COVID-19. During the first wave of vaccination, few working people had the bodily freedom to decide for themselves if they wanted to receive experimental COVID-19 vaccines. The people certainly did not have the right to economic freedom by resisting the requirement of the various medico-political and economic establishments. Freedom of medical inquiry was vitiated by the imperatives of the vaccine mandates, while repurposing approved drugs was actively discouraged. The validity of clinical experience and intuition of primary care physicians (internists, family physicians, pediatricians) was ignored.
None of this is meant to imply that unthinking adoption of any drug in the absence of evidence it may work would be a reasonable path. Neither is vaccine resistance the proper response to a global medical emergency in which vaccines have not worked as hoped. Vaccines still work, just as they did more than 300 years ago to prevent smallpox through variolation, a practice deeply embedded in folk medicine in Asia.
As I wrote in an unpublished review of mRNA vaccines in December 2020:
While the science leading to mRNA vaccines is not experimental, the patent experimental nature of both SARS-CoV-2 mRNA vaccines has not been discussed, very much, in public. If mRNA vaccines turn out to be ineffective, the backlash will be severe. During the current pandemic, citizens of the world have been asked repeatedly to “trust the science” (added note: often by those who have identified themselves with science). Yes. But trustees of science, including politicians, practicing scientists and physicians, and scientist-administrators at NIH/FDA/CDC and their counterparts in other nations, must at all times be careful, especially when working rapidly and under great pressure, to avoid overselling what can be done as what must be done. These mRNA vaccines are commercial products projected to return tens of billions of dollars to their manufacturers in the very near term. Eli Lilly received about $320 million, adjusted for inflation, in the first year of the Salk vaccine.
Alas, trust of and in science has reached its nadir, and the COVID-19 backlash has been responsible most recently. We were even trolled during the past few days that the polio vaccine could be withdrawn (this will never happen and has since been denied by the President Elect). The community of biomedical scientists are responsible for the loss of scientific authority because they have not paid close attention to what has been done in the name of science.
However, it should be noted that HIV/AIDS appeared before Biomedical Science had been transformed into what I have called Biomedicine, the amalgamation of Big Pharma and Big Medicine that was facilitated by the Bayh-Dole Act of 1980.
The continuing aftereffect of Bayh-Dole is that disinterested biomedical research has been effaced by “interested research” at every level. The neoliberalization of science along with everything else proceeds apace, and the market is now the measure of all things in the practice of biomedical science, the funding of biomedical science, and the publication of biomedical science. Philip Mirowski was the first and the best to describe this in his Science-Mart: Privatizing American Science.
One need only compare the scientific literature of HIV/AIDS with that of COVID-19 to appreciate this. As of 17 December 2024, the query “HIV AIDS” retrieves 183,788 results from 1982 through 2024 when searching PubMed, or ~4300 publications per year for 43 years. This is a substantial body of work. “Covid” (case independent) gets 451,098 hits over the past five (5) years, or more than 90,000 “publications” per year. This is a large, mostly insubstantial body of work.
From this one can conclude what has been obvious for some time: The neoliberal hive mind, scientific and otherwise, is very busy but gets very little accomplished. Still, we have done better, as with HIV/AIDS, although much is left to accomplish. We can do better, with COVID-19, too. And beyond.
Notes
This essay is dedicated to the memory of TEP (1952-1991), who was an athlete, artist, landscape architect, friend and mentor, each at a very high level. You are deeply missed but never forgotten. Thank you to GM for providing references during discussions of COVID-19. Needless to say, I am solely responsible for the deficiencies of this essai.
[1] For example, John Keats at the age of 25 in 1821.
[2] Excerpt from this timeline. June 5: The U.S. Center for Disease Control (CDC) publishes an article in its Morbidity and Mortality Weekly Report (MMWR): Pneumocystis Pneumonia—Los Angeles. The article describes cases of a rare lung infection, Pneumocystis carinii pneumonia(PCP), in five young, previously healthy gay men in Los Angeles. Los Angeles immunologist Dr. Michael Gottlieb, CDC’s Dr. Wayne Shandera, and their colleagues report that all the men have other unusual infections as well, indicating that their immune systems are not working. Two have already died by the time the report is published and the others will die soon after. This edition of the MMWR marks the first official reporting of what will later become known as the AIDS (Acquired Immunodeficiency Syndrome) epidemic.
[3] For example, molecular cloning of one gene was still a major project that often required years. My first cloning project began in earnest in 1989, and the paper was published in 1992. This was probably a bit slower than in larger laboratories but it was well within normal. Manual determination of the DNA sequence of the cloned product could take as much as one year of near-daily labor, which my research partner did. He is rightfully the first author on the paper, which at last count had been cited more than 500 times. Today the time required to determine a similar DNA sequence can be measured in hours. The signal technique that revolutionized molecular biology, PCR, was not described until 1986. The small independent biotech firms that made molecular biology feasible at scale had not begun to have an outsized impact before 1986, with the exception of New England Biolabs (which is one of only two independents to my knowledge that remain independent; Bio-Rad is the other), in the early days of HIV/AIDS
[4] “Consumer” has been correctly identified as the Neoliberal term for “citizen.” Here it is doing double duty as the Neoliberal term for “patient” in need. One might also add that while these are “useful new products,” they are not “consumer products.”
[5] From the article, which may be behind a paywall for those without a subscription to the NYT: Gilead charges $42,250 per patient per year for lenacapavir in the United States, where it is approved as a treatment for H.I.V. The company has said nothing about what lenacapavir will cost when used to prevent H.I.V. infections, a process called pre-exposure prophylaxis, or PrEP. The generics makers — three in India, one in the United States, one in Pakistan and one in Egypt.” — are expected to sell it for much less. Researchers at Liverpool University found the drug could profitably be produced for as little as $40 per patient per year, if it were being purchased in large volumes.
[6] For example, UC-Berkeley molecular biologist Peter Duesberg’s insistence that AIDS was not an infectious disease but was caused by the use of amyl nitrite (poppers) as a recreational drug in the gay community. This was an odd thing at the time and has remained so. It was thoroughly discussed in several journal clubs I attended. Duesberg had been a pioneer in showing that viral oncogenes – normal cellular genes hijacked by viruses –can cause cancer in humans when they are inappropriately expressed. He was elected to the National Academy of Sciences based on this research.
[7] CAFO: Concentrated Animal Feeding Operation